Maintaining strong and healthy bones is essential at every age. At Ortho Plus Care, we provide the Best Bone Mineral Density in Sector 51, Gurugram, helping patients detect bone loss early and prevent serious conditions like osteoporosis.
If you’ve ever wondered whether you should get a BMD test, this guide will help you understand who needs it, when to get it, and how Ortho Plus Care ensures accurate and reliable results.
For fast information, contact us on WhatsApp.
Understanding Bone Mineral Density (BMD)
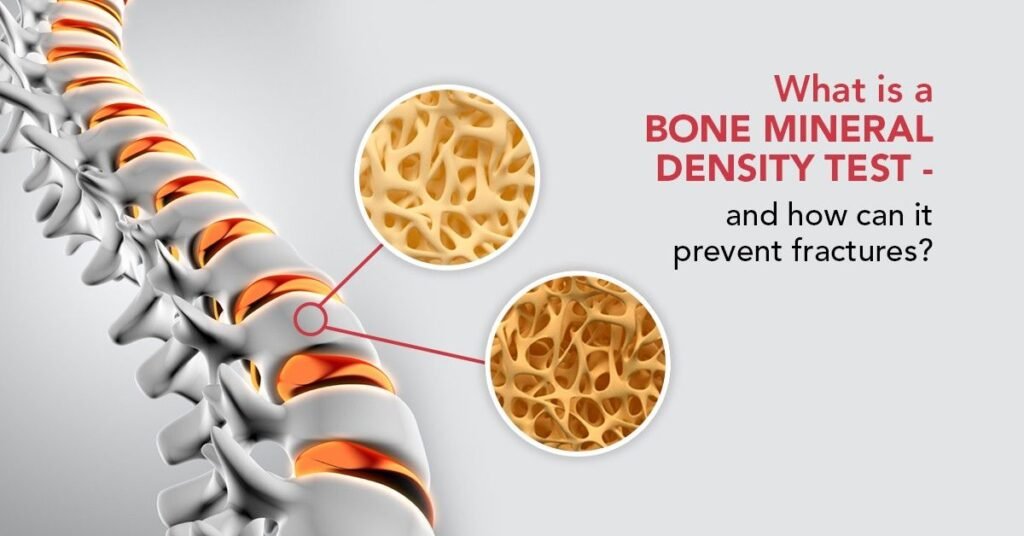
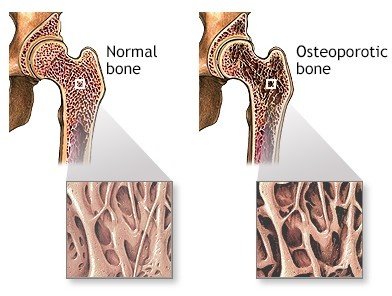
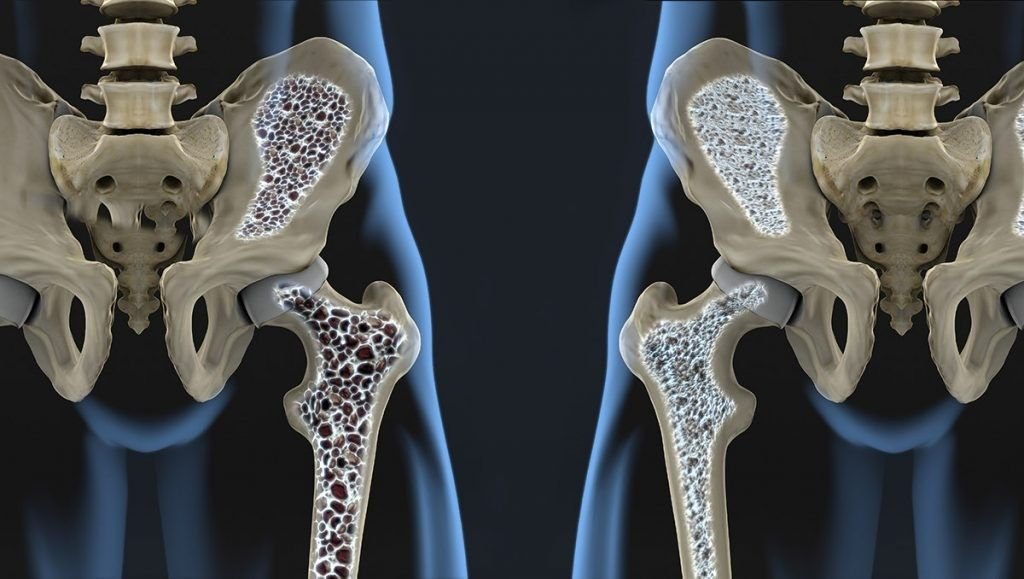
Bone Mineral Density (BMD) measures the amount of minerals, such as calcium and phosphorus, in your bones. A BMD test helps evaluate bone strength and detect conditions that make bones weak or fragile.
At Ortho Plus Care, our advanced diagnostic system offers the Best Bone Mineral Density in Sector 51, Gurugram, using state-of-the-art DEXA scanning technology. This ensures precise results and early detection of even minor bone changes.
Why Bone Health Matters
Bones support your entire body, protect vital organs, and store essential minerals. With age or due to lifestyle factors, bone density naturally decreases. However, excessive bone loss can lead to osteoporosis, fractures, and reduced mobility.
Getting the Best Bone Mineral Density in Sector 51, Gurugram at Ortho Plus Care helps identify early bone loss so you can take preventive action before it becomes serious.
Who Should Consider a Bone Mineral Density Test?
Many people assume bone issues occur only in older adults, but several factors can increase bone loss at any age. You should consider getting tested if you belong to any of the following groups:
1. Postmenopausal Women
After menopause, estrogen levels drop sharply, leading to rapid bone loss. Postmenopausal women are among the highest-risk groups for osteoporosis. Getting the Best Bone Mineral Density in Sector 51, Gurugram helps detect early signs of bone thinning and allows timely intervention.
2. Men Over 50
Although bone loss is more common in women, men also experience gradual declines in bone density after 50. Routine BMD screening can help prevent fractures and bone-related complications.
3. Individuals with a Family History of Osteoporosis
If osteoporosis runs in your family, you may have a higher risk of low bone density. Early screening at Ortho Plus Care ensures preventive care and long-term bone protection.
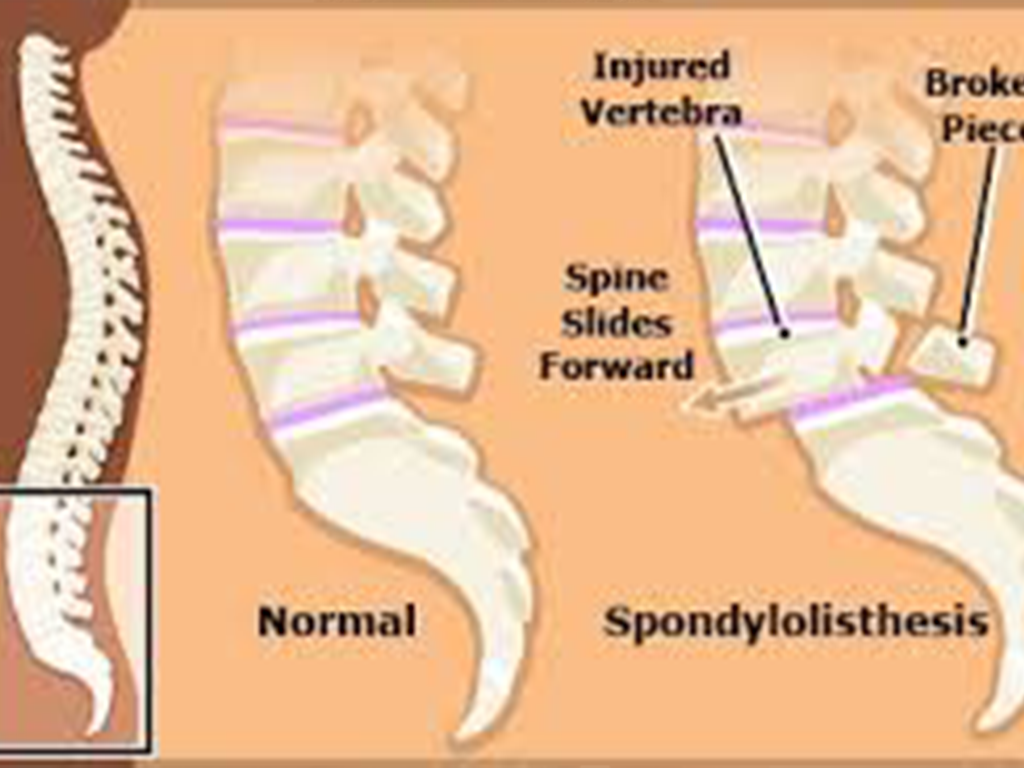
4. People with Frequent Fractures or Bone Injuries
If you experience fractures after minor falls or injuries, your bones may already be weakened. The Best Bone Mineral Density in Sector 51, Gurugram can help identify the underlying cause and guide appropriate treatment.
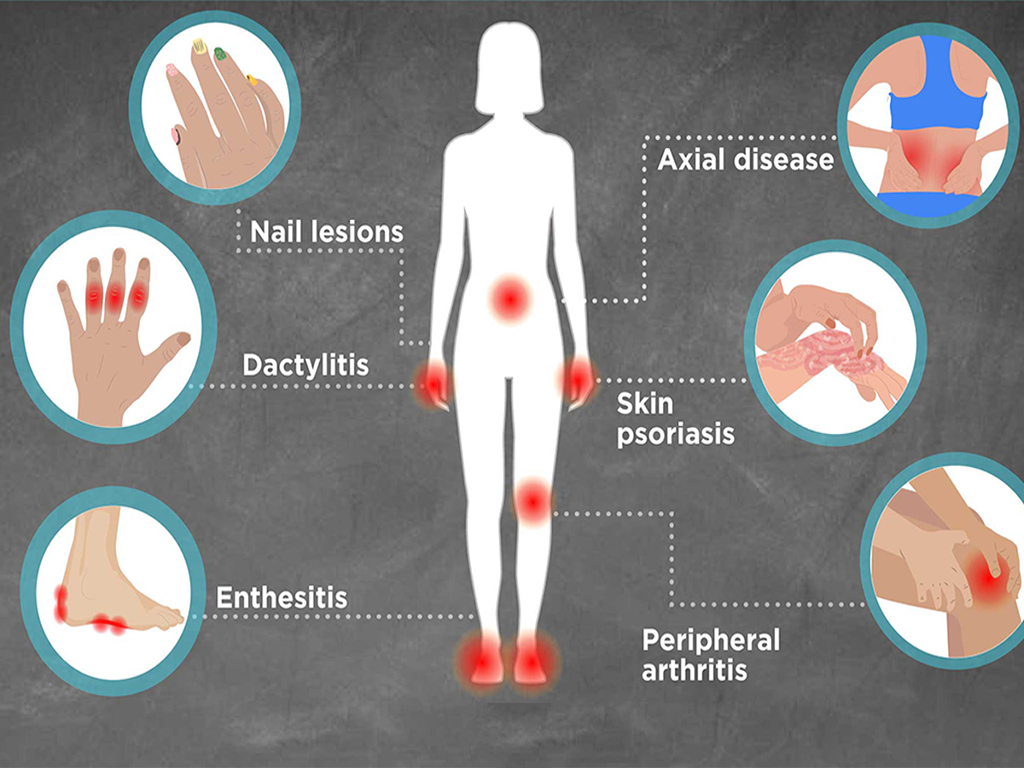
5. Those with Certain Medical Conditions
Medical conditions such as rheumatoid arthritis, thyroid disorders, diabetes, and chronic kidney disease can reduce bone density. If you have any of these, a regular BMD test is essential for monitoring bone health.
6. Individuals Taking Specific Medications
Long-term use of corticosteroids or anti-seizure medications can negatively affect bone strength. Our specialists recommend periodic BMD tests to track bone health and adjust treatment as needed.
7. People with Unhealthy Lifestyle Habits
Smoking, excessive alcohol consumption, and lack of physical activity weaken bones over time. Getting your bone mineral density checked helps identify early bone loss and supports timely lifestyle improvements.
When and Why Should You Get a Bone Mineral Density Test?
Understanding the timing and purpose of a BMD test is key to maintaining lifelong bone health.
When to Get It
- Women aged 65 and above or men aged 70 and above should undergo regular BMD testing.
- Postmenopausal women under 65 with risk factors such as family history or early menopause should be tested earlier.
- Adults over 50 with prior fractures or chronic conditions affecting bone health should also get tested.
- People on long-term steroid therapy or with rapid weight loss may need more frequent monitoring.
Why You Should Get It
A BMD test helps:
- Detect osteopenia or osteoporosis in early stages.
- Assess the risk of future fractures.
- Monitor the effectiveness of osteoporosis treatments.
- Guide nutrition and lifestyle adjustments for stronger bones.
At Ortho Plus Care, offering the Best Bone Mineral Density in Sector 51, Gurugram, our team ensures every test is precise, safe, and tailored to your health profile — empowering you to make informed decisions about your bone health.
The BMD Test Process at Ortho Plus Care
At Ortho Plus Care, we make the testing process simple, comfortable, and highly accurate.
Step 1: Consultation – Our orthopaedic specialist reviews your medical history and risk factors.
Step 2: DEXA Scan – The BMD test uses a painless, non-invasive Dual-Energy X-ray Absorptiometry scanner to measure bone density in the spine, hip, and forearm.
Step 3: Results & Guidance – After analysis, you receive a detailed report along with expert recommendations for maintaining or improving bone health.
Our focus on accuracy and patient comfort makes us the provider of the Best Bone Mineral Density in Sector 51, Gurugram.
Benefits of Early BMD Testing
Early diagnosis through a BMD test offers multiple benefits:
- Early detection of osteoporosis and osteopenia
- Reduced risk of fractures
- Personalized bone health management
- Effective monitoring of treatment progress
- Guidance on calcium and vitamin D intake
By choosing the Best Bone Mineral Density in Sector 51, Gurugram, you take a proactive step toward preventing long-term bone complications.
How Ortho Plus Care Ensures Reliable BMD Results
Ortho Plus Care combines advanced diagnostic technology with expert orthopaedic guidance to deliver the Best Bone Mineral Density in Sector 51, Gurugram.
Here’s why patients trust us:
- Latest DEXA scanning equipment for high-precision results
- Experienced specialists in bone and joint health
- Personalized consultations and risk assessments
- Comfortable, hygienic, and safe testing environment
- Affordable pricing and transparent reporting
Our patient-first approach ensures accurate diagnosis and effective care under one roof.
How Often Should You Get a BMD Test?
The ideal frequency depends on age, risk factors, and existing medical conditions.
- Adults over 50 should get tested every 1–2 years.
- Individuals with osteoporosis or on medications affecting bone health may need more frequent screening.
Our specialists at Ortho Plus Care — known for the Best Bone Mineral Density in Sector 51, Gurugram — will recommend a personalized testing schedule based on your health needs.
Lifestyle Tips to Maintain Healthy Bones
Along with regular testing, adopting healthy habits plays a vital role in improving bone strength:
- Include calcium-rich foods like dairy, leafy greens, and almonds.
- Ensure adequate vitamin D through sunlight or supplements.
- Engage in weight-bearing exercises such as walking or strength training.
- Avoid smoking and excessive alcohol intake.
- Maintain a balanced diet rich in protein and minerals.
At Ortho Plus Care, we not only provide the Best Bone Mineral Density in Sector 51, Gurugram, but also guide patients toward sustainable bone health through holistic lifestyle management.
Conclusion
Bone health often goes unnoticed until problems arise — but with timely diagnosis and preventive care, most bone-related issues can be avoided.
If you are at risk or experiencing signs like frequent fractures, back pain, or posture changes, don’t delay. Visit Ortho Plus Care for the Best Bone Mineral Density in Sector 51, Gurugram, where expert diagnosis meets compassionate care.